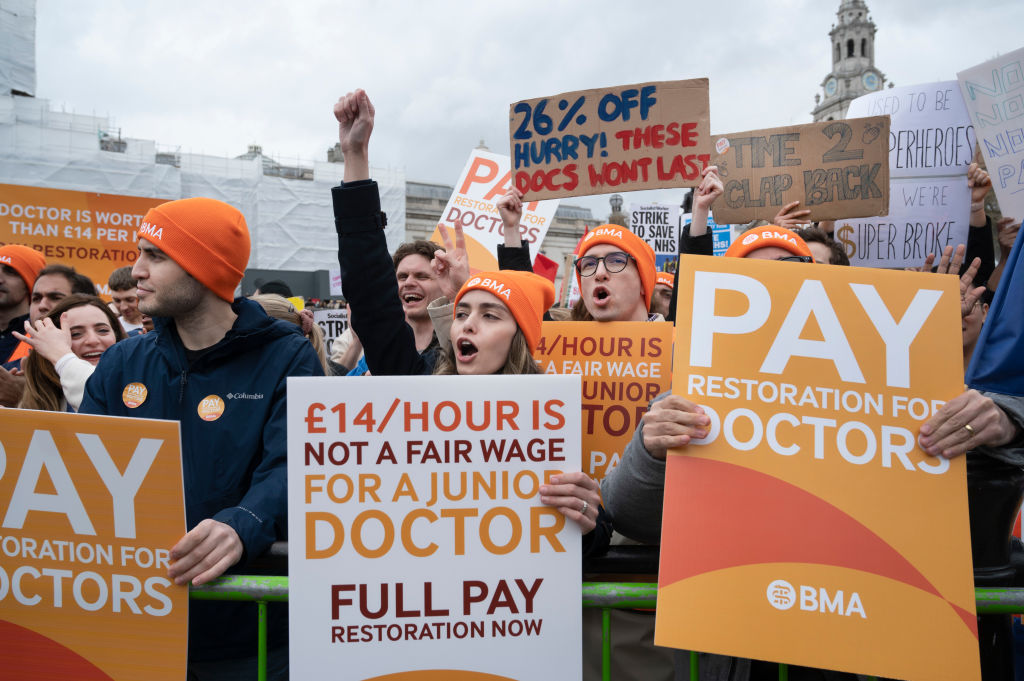
I recently wrote a column elsewhere about the junior doctors strike. As if often the way with this topic, it resulted in some strong and sometimes vituperative reactions.
It also led to many conversations with people in and around medicine. Some of them thought I’d got things wrong. That’s a reasonable position to take, and it’s often useful to take criticism seriously. So I had a think about the column again, and concluded that there were indeed a few things I could have done better at.
Retention
Of the various ‘you’ve got your facts wrong’ critiques of my column, the one I think that has most weight is that I overlook the importance of retention – rather than recruitment – in medicine. In sum, I argued that junior doctors are in a weak bargaining position because the supply of would-be doctors exceeds demand, something that should, in the long run, allow the state to buy more medical labour more cheaply.
I also downplayed the scope for doctors to leave the medical labour market, arguing that they don’t have many alternative buyers for their labour: only a fraction of those who threaten to move to Australia ever do, and employment prospects for doctors outside medicine are not great.
Was I too dismissive? Probably a bit. There is a retention problem. Some doctors do burn out and leave medicine, leaving the NHS short of doctors. That shortfall is around 6 per cent of the total needed. Quite big, but roughly half the shortfall in nurses, which strikes me as a much bigger problem for the NHS. Given that the two groups work in similar settings, I’d suggest that the difference in staffing gaps between doctors and nurses supports my overall point – doctors enjoy better conditions than others, and are in a relatively weak bargaining position – but I still didn’t pay enough attention to burnout/dropout.
The reality of being a junior doctor
I noted in my column that being a doctor means being on a professional conveyor belt that carries you to ever-higher wages and a huge pension, the sort of progression that almost no other workers enjoy. I didn’t reflect on the fact that this leaves junior doctors with few choices and maybe a feeling that they lack agency. Many committed to being doctors in their mid-teens with their A-level choices and other decisions. That constrains their economic and social choices for all of their adult lives, and may help explain the passion they feel around their conditions. I don’t mean to suggest that junior doctors are angry because they’re trapped in gilded cages, but I think I should have thought – and said – more about the experience and outlook of those doctors.
Tuition fees
On that note, I should have mentioned tuition fees. Doctors study for longer and therefore amass more debt. Yes, they’ll pay it back over time (unlike many others who will never earn enough). And that debt is another reason to back my argument for shorter medical training: compressing a five-year medical degree into four years wouldn’t just allow medical schools to train more doctors, it would mean those doctors ran up smaller debts.
But existing debt is still something important to the current cohort of juniors, and I should have raised it.
Rent
Many junior doctors are members of Generation Rent, handing over a huge and painful proportion of their take-home pay on housing they don’t own. That’s not unique to them, and they’re better able than some of their peers to pay such rents. But that doesn’t change the fact that some junior doctors feel their standard of life is harmed by Britain’s miserable housing market. That’s a fair point, and one I should have noted.
I also note that in earlier decades some juniors effectively lived in hospitals, which provided accommodation on site. That was partly because they worked much longer hours – 100-hour weeks were not uncommon – but also reflected a different approach to juniors by their employer. It seems unlikely that the NHS will ever return to housing doctors, but it’s still a topic worth pondering.
My own biases
Before and after publishing that column, I spoke to doctors young and old involved in the strike debate. A caricature of those conversations would be something like this.
Twenty and thirty-something juniors are, like many people of their cohort, angry at what they see as poor conditions, and not afraid to demand better. The people who don’t support them are often older and have enjoyed nice careers, debt-free tuition and a favourable housing market. Damned boomers.
Sixty-something consultants, working and retired, can’t see why today’s juniors are making such a fuss. They have much shorter hours than their predecessors and sometimes better pay. One eminent surgeon showed me evidence that he started his career in the 1970s on a wage worth less than £20k in today’s prices. And for that he was working sometimes twice as long today’s juniors. He, like many of that generation, decided to just grin and bear it. Work is hard, kids. Suck it up.
I’m 47, so I sit between those two age brackets. But I realise that I unconsciously incline towards the ‘suck it up’ side of the argument. For me, unemployment and fear of unemployment are defining facts of my economic life. I grew up in a time and place where losing your job and joining ‘the 3 million’ was a real and terrible prospect.
I think we sometimes forget how significant that fear was. Pop bands used to sing about it. I was a fan of UB40 who were named for a Job Centre claim form and sang ‘I am the one in ten’ about 10 per cent unemployment in the West Midlands.
That all forms my attitude to work and employers, which is quite deferential. Ultimately, they have the power, so at the end of the day, I’m reluctant to be too demanding of more money and better conditions. Don’t rock the boat, because you might go overboard.
Someone who is in their late 20s has had a very different experience of British labour markets and culture. They’ve come of age in a time when the job market is much tighter and unemployment is a much more distant and less frightening concept. Yet at the same time, they haven’t enjoyed the increases in their living standards that people of my age and older did if we got and kept our jobs.
So they feel they have strong reasons for demanding better, and less fear of the consequences of doing so than I or members of my cohort might.
This isn’t just true of junior doctors, of course. It’s something I’ve heard countless times from employers of all sorts in recent years. Younger workers are just more demanding of more from their employers. And while I don’t easily understand that outlook, it exists and I should have tried to explain and analyse it in that column.
Conclusions
I’m not sure how much difference it would have made if I had reflected on the things I’ve listed here in my column. I suspect that junior doctors and others still wouldn’t have liked my central point – that we need to buy more medical labour more cheaply. Even after reflecting here, I still stand by that point. But I accept I should have done more to consider the perspectives and experiences of the people I was writing about. Sorry.




Comments